INTRODUCTION
Cancer is cell growth turned rogue. Advances in surgery and immunotherapy have provided curative treatment options for many common cancers.
Most Asian centres have a department for tumours of each major organ – colorectal, upper gastrointestinal, hepatobiliary, urology, breast surgery and head and neck surgery. However, for rare cancer and cancers that defy organ margins, treatment becomes tricky as available expertise is limited in Asia. Soft tissue sarcomas and peritoneal carcinomatosis are prime examples of cancers that defy organ margins.
THE DEPARTMENT OF SARCOMA, PERITONEAL AND RARE TUMOURS (SPRinT)
At the National Cancer Centre Singapore (NCCS) and Singapore General Hospital (SGH), the Department of Sarcoma, Peritoneal and Rare Tumours (SPRinT) was formed in 2019 in recognition of the growing need for centralised care for advanced and rare cases.
SPRinT is a specialised oncological unit that manages advanced cancers with peritoneal carcinomatosis, soft tissue sarcoma, melanoma and rare tumours with the support of multidisciplinary expertise in a tertiary institution.
SPRinT is comprised of a team of surgeons trained in world-renowned institutes. According to a recently published review of SPRinT in the Asian Journal of Surgery, the outcomes of sarcoma resections and cytoreductive surgeries by SPRinT are comparable to global standards.1

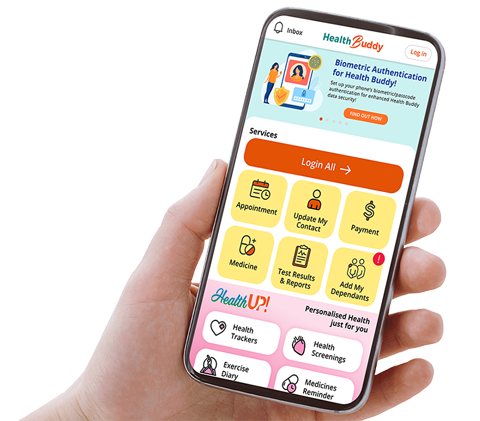
Figure 1. SPRinT – A one-stop surgical centre for advanced and rare malignancies (click to expand infographic)
THE SPRinT SERIES: PARTNERING GPs TO CARE FOR ADANCED AND RARE CANCERS
This is the first in a five-part series of articles, ‘The SPRinT Series’ – in which we will discuss the work that SPRinT does, the key aspects of our clinical focus and the role of general practitioners (GPs) in providing care.
Due to the rarity of these tumours, it is critical for patients to be promptly referred to a specialist department/centre, such as SPRinT, to provide the best outcomes.
GPs are our first line of defence, and close collaboration between SPRinT and the GP community is essential for the timely diagnosis and referral of patients with rare tumours.
FOUR KEY AREAS OF CLINICAL FOCUS
SPRinT has four key focus areas:
- Sarcoma
- Peritoneal surface malignancies
- Rare tumours
- Surgical palliation
Each aspect will be explored further in the subsequent articles of this series.
1. S for Sarcoma
Malignant soft tissue tumours, or sarcomas, are clinically difficult to differentiate from benign lumps such as lipoma. The rarity of this disease coupled with heterogeneity of subtype has led to a unifying consensus that sarcomas are best managed in tertiary units with a multidisciplinary team comprising medical oncologists, specialised sarcoma surgeons, radiation oncologists, pathologists and radiologists well-versed in this disease.
In SPRinT, every sarcoma case is discussed at the sarcoma tumour board within the week. Centralising sarcoma care improves the diagnostic interval because patients do not lose time in the primary care setting or in surgical units with no sarcoma expertise. Patients receive appropriate imaging for tumour staging and get a higher rate of preoperative pathological diagnosis. Targeted treatment is provided in a timely manner, according to recommendations from sarcoma experts in Singapore.
In the next part of the series, we will discuss the role of GPs in early detection and referral of these patients. We will share on the suspicious features to look out for that require a direct referral to SPRinT, as well as why an early referral to a specialised centre is key to achieving the best possible outcome. We will also introduce the multidisciplinary team that looks after these patients.
2. P for Peritoneal Surface Malignancies
Peritoneal surface malignancies refer to a wide variety of cancers that involve the peritoneum. The tumours may arise from the peritoneum or spread to the peritoneum from primary tumours in other organs.
The diagnosis of peritoneal spread from a variety of cancers is becoming increasingly common, even at diagnosis of the primary tumour. What was once considered a terminal condition is now suitable for curative treatment in some patients diagnosed with peritoneal surface malignancy – and if not, there are other treatment options available.
Cytoreductive surgery has been shown to be an effective treatment strategy to reduce disease burden.2-3 In SPRinT, patients have the option of having hyperthermic intraperitoneal chemotherapy (HIPEC) in the same setting as cytoreductive surgery to delay tumour recurrence in the peritoneum.
However, only a small minority of patients are suitable for this treatment. For some others, pressurised intraperitoneal aerosol chemotherapy (PIPAC) is another option to reduce symptoms and slow tumour growth.
The third part of the series will introduce peritoneal surface malignancies and discuss how early referral to a specialised team impacts patient outcomes for these cancers.
3. Surgical Palliation
Time is precious for patients with advanced cancers. Due to widespread disease, these patients are often not candidates for curative treatment, partly due to the highly invasive nature of complex multi-organ resection.
However, in a select group of patients, palliative surgery can serve to both prolong lifespans and improve quality of life by directly eliminating the problem, challenging the current paradigm of palliative care. In patients who have exhausted all possible avenues of treatment, surgical intervention can help alleviate some symptoms, allowing them to live their remaining lives in relative comfort and dignity.
In the fourth part of the series, we will take an in-depth look at the concept of active palliation, the options that SPRinT provides for these patients, and how GPs, who may be caring for the patient even before their cancer diagnosis, can support them on this journey.
4. R.T. for Rare Tumours
Patients with rare tumours can seek surgical care in SPRinT. SPRinT manages rare tumours referred to NCCS. Below are some examples, though the list is not exhaustive.
- Asian subtypes of advanced melanoma
- Advanced squamous cell carcinoma
- Gastrointestinal stromal tumours (GIST)
- Extramammary Paget disease (EMPD)
- Dermatofibrosarcoma protuberans (DFSP)
Treatment of these rare tumours are guided by tumour biology, careful patient selection and discussion by a panel of experts in this field according to the latest international guidelines.
The diagnosis of rare tumours is a crucial and important first step in the journey of these patients. The team at SPRinT works with specialists from multiple disciplines to pull together a collective experience and expertise.
In the last part of the series, we will introduce some of these rare tumours and discuss the role of GPs in early detection and referral of these patients.
THE PATIENT JOURNEY IN SPRinT
All patients referred to SPRinT are seen by specialists in NCCS. SPRinT seeks to provide holistic care for patients with peritoneal disease, sarcomas and other rare tumours through working closely together with other disciplines.
Each case is analysed in depth and discussed comprehensively in multidisciplinary tumour boards comprising experts in surgical oncology, medical oncology, radiation oncology, pathology and radiology according to tumour type.
Timely treatment recommendations are guided by international guidelines and many years of experience. We are also working to raise awareness about rare and advanced malignancies so that patients can be referred in a timely manner to receive the appropriate care.
The journey in fighting cancer is physically and emotionally draining for both patients and caregivers. Patients with advanced cancers who need additional support outside surgical and medical therapy are discussed in weekly palliative tumour board meetings, with rehabilitation practitioners and allied health professionals such as physiotherapists and medical social workers, so that holistic care can be provided to support patients and their caregivers.
CASE STUDY |
|---|
One patient receiving care under SPRinT is a 36-year-old woman who presented with a vague abdominal wall lump for three months. Following an excision biopsy, she was diagnosed with synovial sarcoma, and subsequently referred to SPRinT. The patient's condition, prognosis as well as her concerns were discussed at a multidisciplinary meeting comprising SPRinT surgeons, plastic surgeons, medical oncologists and pathologists. The surgical team promptly performed a wide excision with a free flap. Adjuvant chemotherapy was offered and the patient is currently disease-free and under routine surveillance by the SPRinT team. |
REFERENCES
- Tu IWH, Wong JSM, Tan QX, Ng G, Ong C-AJ, Chia CS. Department of Sarcoma, Peritoneal and Rare Tumors (SPRinT): A Subspecialty Surgical Oncological Care Model for Advanced Malignancies Requiring Complex Procedures. Asian Journal of Surgery. 2021; S1015-9584(21)00601-1
- Kusamura S, Baratti D, Deraco M. Multidimensional analysis of the learning curve for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in peritoneal surface malignancies. Annals of surgery. 2012; 255(2):348-56.
Smeenk R, Verwaal V, Zoetmulder F. Learning curve of combined modality treatment in peritoneal surface disease. British Journal of Surgery. 2007; 94(11):1408-14.
For GP referrals to the Department of Sarcoma, Peritoneal and Rare Tumours (SPRinT), please contact NCCS at:
Hotline: 6436 8288 Click here for more information on the department. |