National Cancer Centre Singapore will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
Nail Changes
- Allergies
- Appetite Loss
- Bone Problems
- Breathing Problems
- Constipation
- Diarrhoea
- Difficulty Swallowing (Dysphagia)
- Dry Mouth (Xerostomia)
- Difficulty Sleeping (Insomnia)
- Feeling Tired (Fatigue)
- Fevers and Infections
- Hair Loss
- Heart Problems
- Menopausal Symptoms
- Indigestion
- Joint Pains
- Limb Swelling (Lymphedema)
- Muscle Aches
- Nail Changes
- Nausea and Vomiting
- Pain
- Tingling or Numbness in Hands or Feet (Peripheral Neuropathy)
- Skin Changes
- Sore Mouth (Oral Mucositis)
- Taste Changes

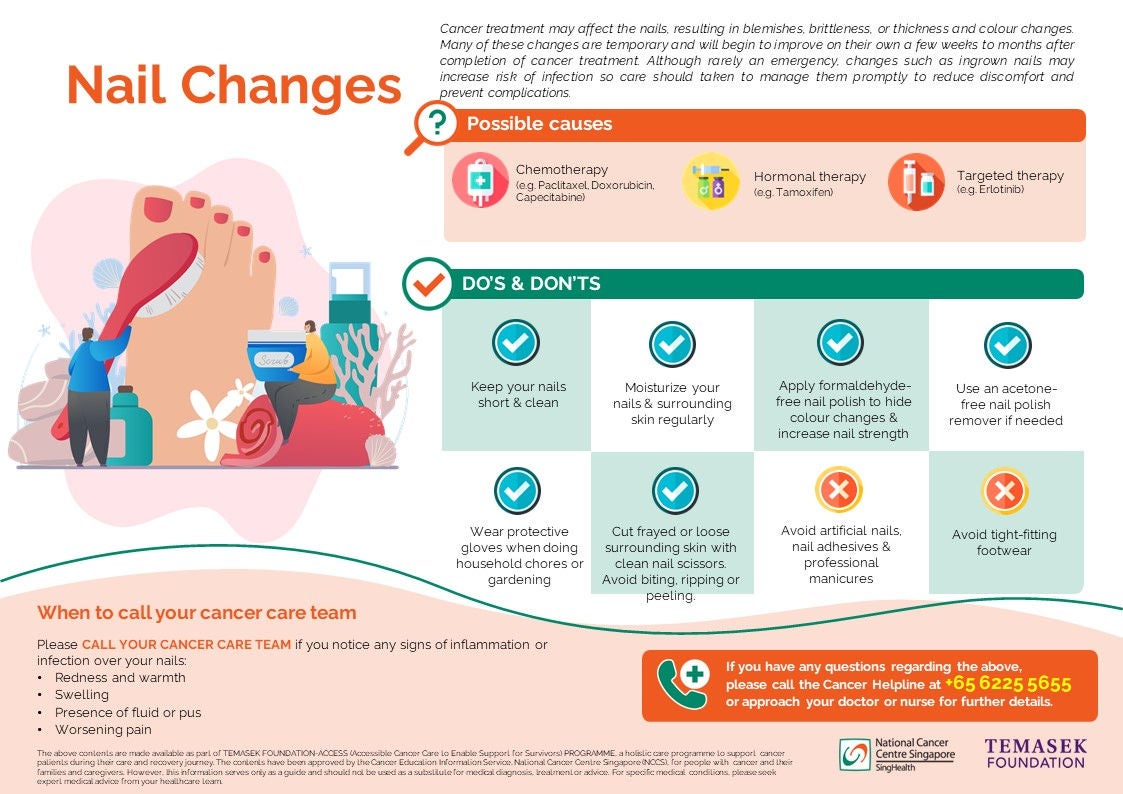
Cancer treatment can affect the fast-growing cells in your nails, leading to changes in the fingernails or toenails. Although the severity differs from person to person, nail changes may be visible and uncomfortable, and can at times affect your daily activities such as buttoning your shirt. Examples of nail changes include nail breakages, darkening, surrounding swelling and redness. Many of these changes begin to improve a few weeks after the completion of treatment, but care should be taken during the treatment phase to decrease discomfort and prevent complications.
Causes of Nail changes
Some cancer treatment are more likely to cause nail changes than others. These include:
- Chemotherapy, particularly taxanes (e.g. paclitaxel, docetaxel), anthracyclines (e.g. doxorubicin) and Capecitabine or 5-Fluorouracil.
- Hormonal therapy, namely tamoxifen.
- Targeted therapies, particularly EGFR inhibitors (e.g. Erlotinib).
What you need to look out for
Not all people will experience nail changes, but if you do, they usually occur about 3-6 weeks after starting cancer treatment. Some of them may include:
- Weak, brittle nails that tend to break or crack more easily
- Nail colour changes: darkening or changes in color (e.g. to yellow or brown)
- Changes in nail thickness, shape or texture
- Nail separation from nail bed
- Line marks, grooves or ridges along the nail
- Red, painful or frayed surrounding skin
- Development of ingrown nails
- Slow nail growth
Unlike those caused by chemotherapy, nails changes caused by targeted therapies usually come in the form of nail fold infections (paronychia) and red skin growths around the nails that bleed easily (pyogenic granulomas).
How it can be treated
Most nail problems are temporary, and should heal within a few weeks. Marks on nails will grow out in time. Taking care of your nails to prevent complications is the best treatment for nail problems (see section on “What you can do” below). If you develop a bacterial or fungal infection around your nails, your doctor may prescribe you with antibiotic or antifungal therapy.

What you can do
The following are some of the do’s and don’ts to help you manage nail changes, as well as prevent further complications:
Prevent nail damage
|
|
Prevent infection
|
|
When to call your cancer care team
Please inform your doctor or nurse as soon as you notice any signs of inflammation or infection over your nails:
- Redness and warmth
- Swelling
- Draining fluids or pus
- Worsening pain
If you have any questions regarding the above information, please call Cancer Helpline at +65 6225 5655 or approach your doctor or nurse for further details.
Click here to download the PDF version of this article.
如果您要下载本文的中文版本,请点击此处。
Klik di sini untuk memuat turun versi PDF artikel ini.
The above contents are made available as part of TEMASEK FOUNDATION-ACCESS (Accessible Cancer Care to Enable Support for Survivors) PROGRAMME, a holistic care programme to support cancer patients during their care and recovery journey.
The contents have been approved by the Cancer Education Information Service, National Cancer Centre Singapore (NCCS), for people with cancer and their families and caregivers. However, this information serves only as a guide and should not be used as a substitute for medical diagnosis, treatment or advice. For specific medical conditions, please seek expert medical advice from your healthcare team.
Brought to you by:
![]()
![]()
Keep Healthy With
© 2025 SingHealth Group. All Rights Reserved.