National Cancer Centre Singapore will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
Skin Changes
- Allergies
- Appetite Loss
- Bone Problems
- Breathing Problems
- Constipation
- Diarrhoea
- Difficulty Swallowing (Dysphagia)
- Dry Mouth (Xerostomia)
- Difficulty Sleeping (Insomnia)
- Feeling Tired (Fatigue)
- Fevers and Infections
- Hair Loss
- Heart Problems
- Menopausal Symptoms
- Indigestion
- Joint Pains
- Limb Swelling (Lymphedema)
- Muscle Aches
- Nail Changes
- Nausea and Vomiting
- Pain
- Tingling or Numbness in Hands or Feet (Peripheral Neuropathy)
- Skin Changes
- Sore Mouth (Oral Mucositis)
- Taste Changes

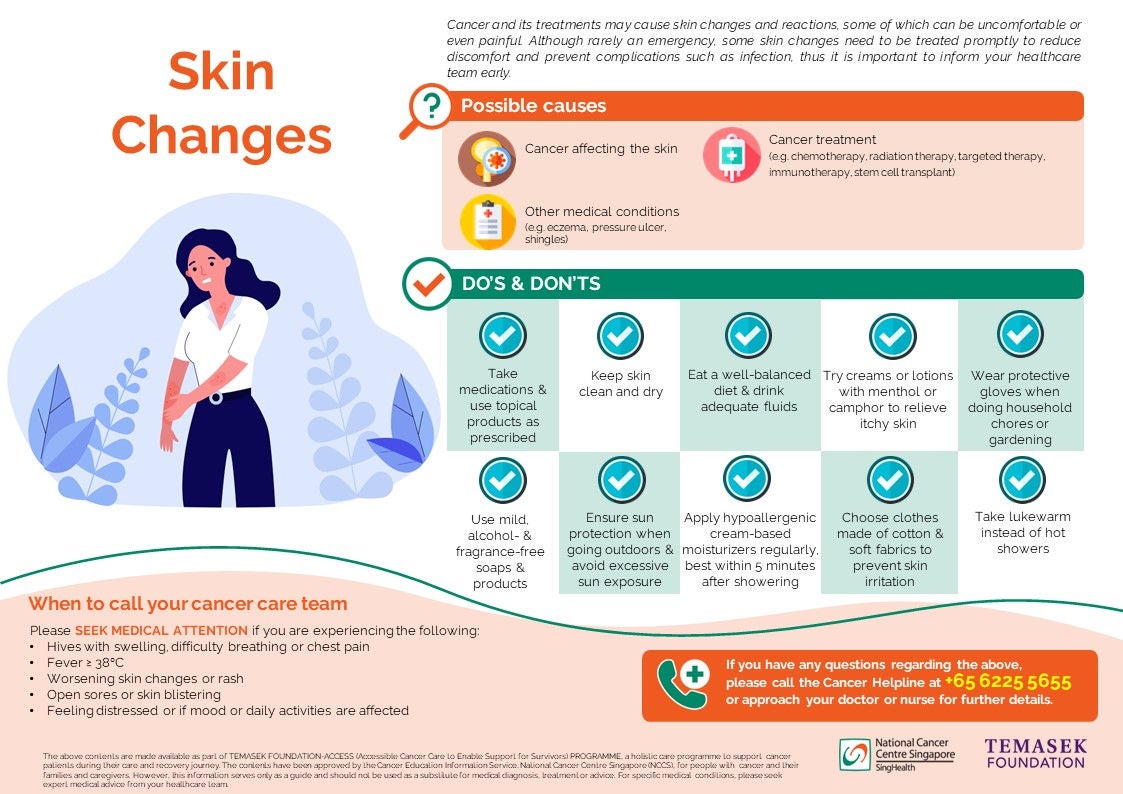
Cancer treatments may cause different types of skin changes and reactions, which could be a source of discomfort and pain. Although skin changes are usually mild and will improve once treatment completes, some may be potentially serious or can cause long-term damage. However, not all changes are negative and certain rashes are actually associated with better response to cancer treatment. It is thus important to inform your doctor or nurse once you notice any skin changes or reactions, so that they can be assessed and treated promptly.
Causes of Skin changes
- Chemotherapy. Chemotherapy targets the fast-growing cells in our bodies, and these include our skin cells. Changes can occur over any area of the body (e.g. darkening of the skin under your nails). At times, skin changes can indicate an allergic reaction to the chemotherapy drug received.
- Radiation therapy. Skin changes for people undergoing radiation therapy usually occurs over the part of the body that is receiving radiation, after 1-2 weeks of treatment. They usually improve a few weeks after treatment ends.
- Targeted therapy. Acne-like rashes on the face and upper body may occur within the first few weeks of taking certain types of targeted therapy, together with other skin-related problems like dryness, itch and increased sensitivity to sunlight. Examples of targeted therapy drugs that cause skin changes include: Afatinib, Cetuximab, Erlotinib, Everolimus, Gefitinib, Lapatinib, Osimertinib, Panitumumab, Sorafenib, Sunitinib, and Vemurafenib.
- Immunotherapy. Skin changes caused by immunotherapy depends on the specific drug received, and may include itch, redness, blistering or yellowing of the skin and eyes. Common immunotherapy drugs that cause skin-related problems are: Nivolumab, Pembrolizumab, Atezolizumab, Ipilumimab.
- Graft versus host disease. Graft versus host disease, a complication after stem cell transplant whereby the donor cells recognises the body’s own cells as foreign and attacks them, can lead to skin problems like rashes and blisters.
- Prolonged pressure. Difficulties in moving about can lead to constant pressure on certain areas of the body, and this can cause pressure skin ulcers to form. The tailbone, ears and heels of the feet are common areas of pressure skin ulcers, as there are lesser fats over those areas. Prevention is key to the management of pressure skin ulcers, and prompt treatment is important to reduce discomfort and prevent them from getting worse.
- Cancer. Cancer sometimes can break the skin and cause wounds that are called “malignant wounds”. Problems associated with these wounds include odour, bleeding or fluid leakages. Speak to your nurse if you have a malignant wound – he or she will be able to advise you on how best to manage the wound.
What you need to look out for
Depending on your condition and the type of cancer treatment you are receiving, skin changes that you may experience can include:
- Dry, peeling or flaky skin
- Redness
- Itch
- Photosensitivity (increased sensitivity to sunlight, getting sunburns more easily)
- Hyperpigmentation (development of dark patches or generalised darkening of skin)
- Discoloration over vein where chemotherapy was administered
- Rashes (Acne-like or any form of inflamed, irritated or swollen skin)
- Hives (Raised, itchy skin rashes)
- Blistering or wet sores
- Burning or pain over skin changes
- Broken skin over pressure areas
- Tingling or numbness in palms or soles
How it can be treated

Treatment will depend on the cause and severity of your skin problems, as well as any associated symptoms you may experience. These may include:
- Skin care advice (see section on “What you can do” below)
- Medicated skin creams (e.g. creams containing corticosteroids) to relieve your discomfort
- Antibiotic treatment if there are signs of infection
- Antihistamines (e.g. Zyrtec) to treat allergic reactions and help relieve generalised itch
- Painkillers if pain is present
Your doctor will also decide on whether there is a need to adjust your treatment, particularly if you experience more serious skin reactions and problems. If necessary, you may be referred to a dermatologist, who specializes in managing skin conditions.
What you can do
Although some skin changes cannot be avoided entirely, there are things you can do to reduce uncomfortable symptoms and prevent complications. Even before starting any cancer treatment, start moisturizing and protecting your skin on a regular basis. The following are some other steps you can take:
|
|
When to call your cancer care team
Please inform your doctor or nurse if you notice or experience any of the following:
- Signs of an allergic reaction: hives accompanied by swelling, difficulty breathing or chest pain. You should seek medical attention immediately if these occur
- Signs of infection: fever of > 38 degree celsius, chills or rigors
- Worsening skin changes or rash
- Uncomfortable symptoms affecting daily activities or sleep (e.g. itch, pain)
- Open sores or blistering over skin
If you have any questions regarding the above information, please call Cancer Helpline at +65 6225 5655 or approach your doctor or nurse for further details.
Click here to download the PDF version of this article.
如果您要下载本文的中文版本,请点击此处。
Klik di sini untuk memuat turun versi PDF artikel ini.
The above contents are made available as part of TEMASEK FOUNDATION-ACCESS (Accessible Cancer Care to Enable Support for Survivors) PROGRAMME, a holistic care programme to support cancer patients during their care and recovery journey.
The contents have been approved by the Cancer Education Information Service, National Cancer Centre Singapore (NCCS), for people with cancer and their families and caregivers. However, this information serves only as a guide and should not be used as a substitute for medical diagnosis, treatment or advice. For specific medical conditions, please seek expert medical advice from your healthcare team.
Brought to you by:
© 2025 SingHealth Group. All Rights Reserved.